Universal Occupational Licensing Recognition and Healthcare Access
Healthcare shortages in some regions of the United States have prompted policymakers to seek ways to redistribute physicians. Reducing regulatory barriers limiting interstate practice has been highlighted as one way to improve regional healthcare access and patient outcomes.
In Does Universal Occupational Licensing Recognition Improve Patient Access? Evidence from Healthcare Utilization (NBER Working Paper 34030), researchers Yun taek Oh and Morris M. Kleiner examine whether Universal Licensing Recognition (ULR)—a policy that allows out-of-state physicians to practice without relicensing—affects healthcare utilization.
Universal occupational licensing recognition allows physicians from any state to practice without relicensing, increasing patient access to personal doctors and reducing cost barriers.
The researchers distinguish ULR from the Interstate Medical Licensure Compact (IMLC), which only facilitates license portability between participating states. ULR is more comprehensive. Because it recognizes licenses from any US state, it potentially expands the pool of available physicians. While the IMLC covers about 80 percent of US physicians, ULR could enable the remaining 20 percent to practice across state lines without lengthy relicensing processes.
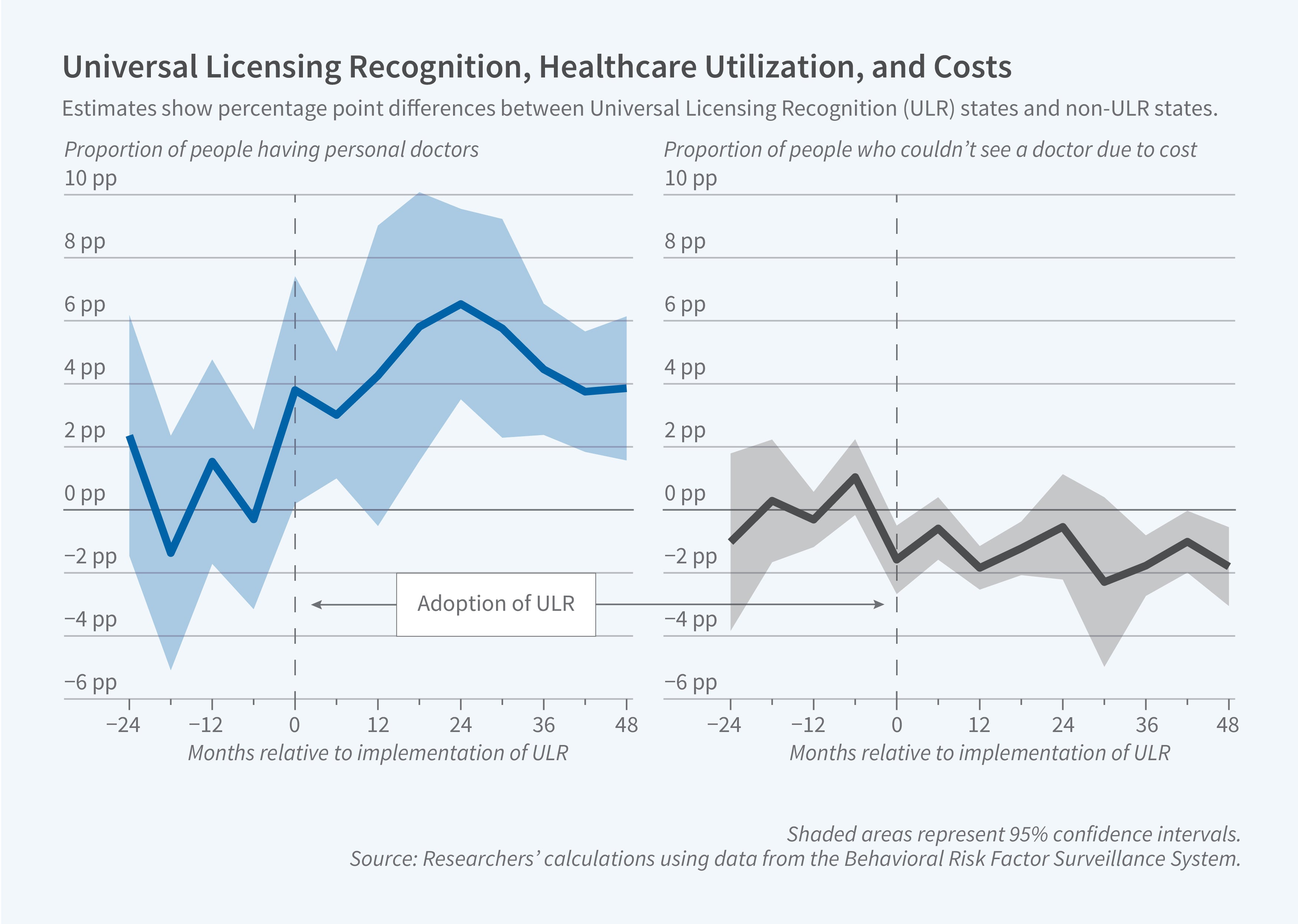
Using data from the Behavioral Risk Factor Surveillance System from 2018 to 2023, the researchers measure how healthcare utilization changed after states adopted ULR. They supplement this with data from IPUMS USA, IPUMS CPS, and the Centers for Medicare & Medicaid Services to examine changes in physician mobility and practice patterns.
The proportion of individuals with personal doctors or healthcare providers significantly increased in states that adopted ULR. This effect was particularly pronounced among older individuals (ages 45–64) and seniors (ages 65–79), populations with higher healthcare needs. There was also a significant reduction in the proportion of individuals who reported not seeing a doctor due to cost constraints.
The researchers did not find any significant increase in interstate migration of physicians following ULR adoption. Instead, expanded healthcare access came through increased use of out-of-state practices—physicians practicing across state lines without relocating, including temporary and telehealth physicians. Interestingly, states that adopted ULR but imposed residency requirements showed no significant rise in healthcare utilization, suggesting that such requirements effectively nullified the effects of license recognition.
The researchers find that the observed expansions in healthcare access were specifically attributable to universal reciprocity of physician licenses rather than other factors related to ULR adoption. The effects remained consistent even when controlling for Medicaid expansion and other potentially confounding factors. The findings suggest that ULR can affect the regional distribution of physicians and increase healthcare access without requiring physical relocation of the workforce.


