Opioid Use by SSDI Beneficiaries and the Effect of Opioid Prescribing on SSDI Claiming
Chronic pain is a leading cause of work disability and a primary reason for receipt of SSDI benefits. Prescription opioids are frequently prescribed for chronic pain, but their use has been scrutinized in recent years due to concerns about addiction and overdose. Understanding how common prescription opioid use is among SSDI beneficiaries and how opioid use affects employment and SSDI applications is critical to the SSDI program.
Researchers Nicole Maestas, Tisamarie Sherry, and Alexander Strand explore these issues in a pair of new working papers. In Opioid Use among Social Security Disability Insurance Applicants, 2013–2018 (NBER RDRC Working Paper NB19-28-1), the three researchers estimate the prevalence of opioid use among SSDI applicants at the time of application.
Developing national estimates of the prevalence of opioid use among SSDI applicants has proved challenging. Social Security’s electronic disability database allows applicants to indicate prescription opioid use by selecting it from a pre-populated drop-down list or by entering it as free text — however, the free text information is difficult for analysts to use. The authors use a novel natural language processing algorithm to identify opioid analgesics in free text entry fields and apply this approach to administrative records for all SSDI applicants who submitted a claim between 2013 and 2018.
They find that the prevalence of opioid use among SSDI applicants declined from 33 percent in 2013 to 24 percent in 2018. By contrast, the share of applicants reporting musculoskeletal impairments, which are commonly associated with chronic pain, was unchanged during this period. Reported opioid use declined across both sexes, all age groups, and all education levels. Use declined across all regions, though the Midwest and Southeast had the smallest decreases. Intriguingly, communities that had higher levels of opioid prescribing or smaller declines in prescribing over time also had higher levels of SSDI applications overall and more applications reporting opioid use.
This observation motivates a second paper by Maestas and Sherry, Opioid Treatment for Pain and Work and Disability Outcomes: Evidence from Health Care Providers’ Prescribing Patterns (NBER RDRC Working Paper 19-28-2). This paper explores how higher rates of opioid prescription in an area affect employment outcomes and SSDI applications. On the one hand, opioid use may help individuals to control chronic pain, leading to higher employment and fewer SSDI applications. On the other hand, adverse medical consequences of opioid use — including but not limited to dependence and addiction — might have the opposite effect. Moreover, increased opioid supply in a given area could negatively affect the labor supply of individuals who are not experiencing pain if it increases recreational drug use and addiction.
A fundamental challenge of estimating the relationship between opioid use and labor outcomes is that opioids are prescribed for chronic pain and areas where individuals experience more pain may have other attributes that lead to less work and more SSDI applications. To surmount this challenge, the authors use variation in health care providers’ opioid prescribing preferences — like the tendency to prescribe drugs at higher dosages and for longer durations — that are not explained by patient characteristics. They leverage the largest available US commercial claims database to construct a measure of opioid prescribing propensity that is independent of patients’ medical and demographic characteristics and labor force attachment. This approach also mitigates the concern that “doctor shopping” by patients seeking opioids might blur the relationship between opioid use and other outcomes.
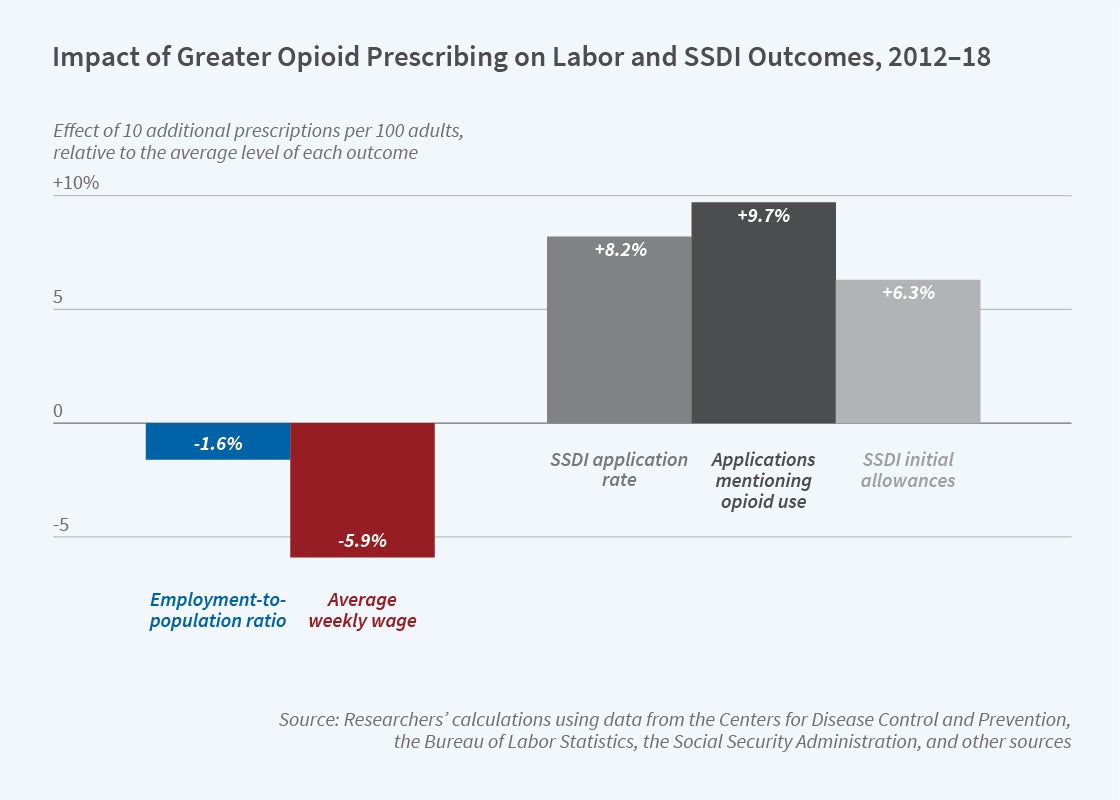
The authors find that in areas with a higher opioid prescribing propensity, employment and wages are lower. Specifically, 10 additional opioid prescriptions per 100 adults in a local area lead to a 1.6 percent decrease in employment and a 6 percent decrease in the average weekly wage, relative to the sample average. Further, an increase of 10 prescriptions per 100 adults is associated with an 8 percent increase in SSDI applications, a 10 percent increase in applications mentioning opioid use, and a 6 percent increase in the probability that an application is allowed at the initial review, relative to mean values.
The authors conclude “[o]ur findings indicate that opioid treatment for pain can have adverse effects on labor productivity and employment, even precipitating more permanent separation from the labor force through SSDI claiming.…[W]here medically possible, decreased reliance on opioid analgesics for pain treatment (and possibly increased use of effective non-opioid pain therapies with fewer adverse effects) can not only improve patients’ health, but also work-related functioning and labor outcomes.”
The research reported herein was performed pursuant to grants DRC12000002-05 and RDR18000003 from the US Social Security Administration (SSA), funded as part of the Retirement and Disability Research Consortium, from grant P01AG005842 from the National Institute on Aging, and a gift from Owen and Linda Robinson. The opinions and conclusions expressed are solely those of the author(s) and do not represent the opinions or policy of SSA, any agency of the Federal Government, or NBER. Neither the United States Government nor any agency thereof, nor any of their employees, makes any warranty, express or implied, or assumes any legal liability or responsibility for the accuracy, completeness, or usefulness of the contents of this report. Reference herein to any specific commercial product, process or service by trade name, trademark, manufacturer, or otherwise does not necessarily constitute or imply endorsement, recommendation or favoring by the United States Government or any agency thereof.


