Changes in Infant Health in Response to Hospital Breastfeeding Support Policies
The World Health Organization and the American Academy of Pediatrics recommend that infants be exclusively breastfed for the first six months of life and continue breastfeeding through at least one year of age. To promote these practices, sixteen US states as of 2022 had adopted hospital regulations requiring specific care standards during the postpartum hospital stay. These policies typically mandate that hospitals employ lactation consultants, train staff in breastfeeding support, inform mothers about breastfeeding benefits, and allow newborns to room-in with mothers 24 hours per day.
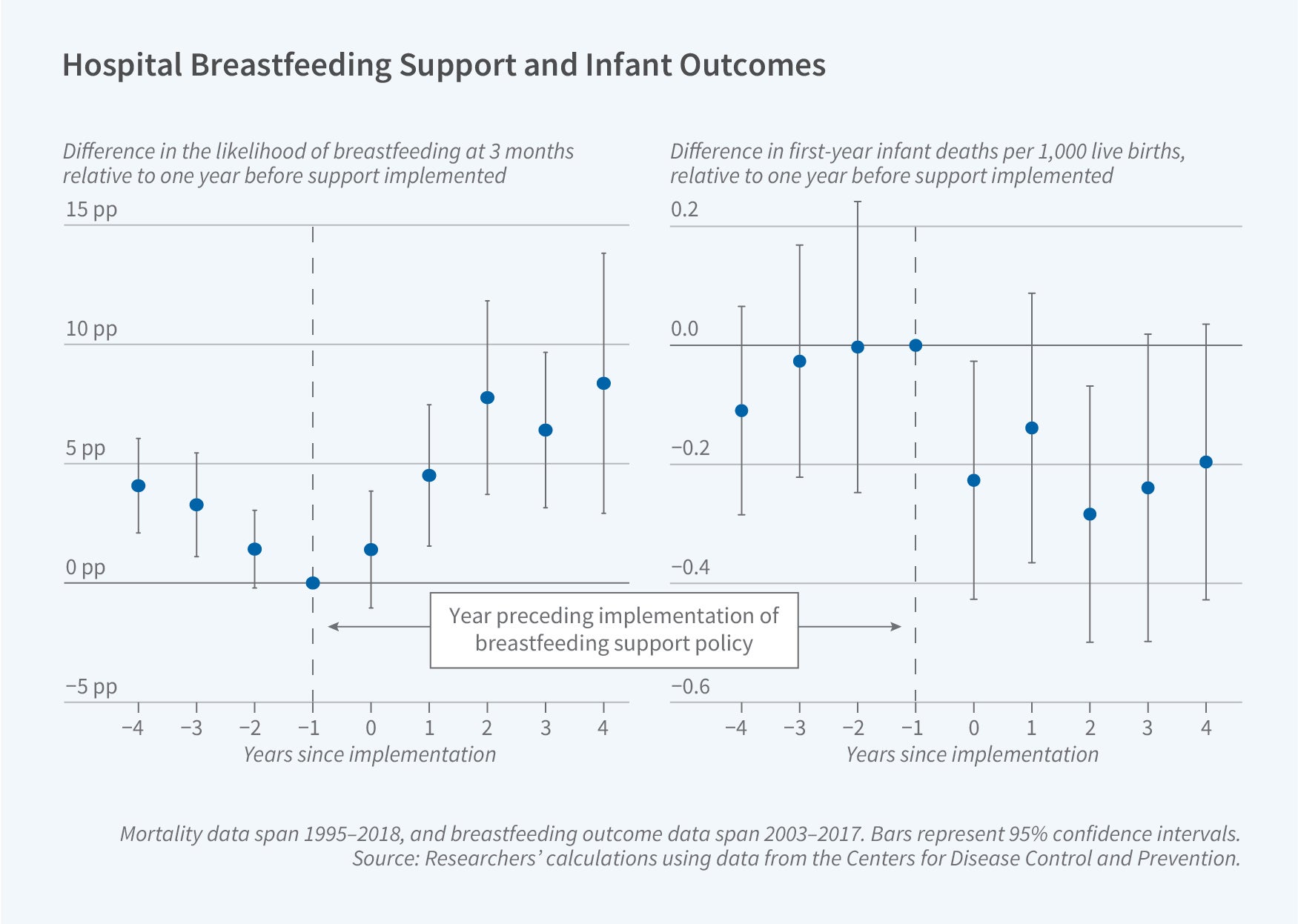
In The Effect of Hospital Breastfeeding Policies on Infant Health (NBER Working Paper 34032), Emily C. Lawler and Meghan M. Skira examine whether these breastfeeding support policies improve infant health. They analyze data from 1995 to 2018 for mortality outcomes and from 2000 to 2019 for inpatient hospitalization outcomes, leveraging variation in the timing of state policy adoption. They estimate that these regulations reduced infant mortality by approximately 3.5 percent, averting an estimated 2,090 infant deaths.
The implementation of state breastfeeding support policies in US hospitals improved infant health outcomes.
They find that following policy adoption, first-year infant mortality declined by 0.22 deaths, with reductions occurring in both the neonatal (0.10 deaths) and postneonatal (0.11 deaths) periods. In the full sample, there were, on average, 6.5 deaths within the first year of life per 1,000 births—4.3 deaths within the first 28 days (the neonatal period) and 2.2 deaths between 28 and 364 days (the postneonatal period).
These mortality reductions were concentrated among the most vulnerable infants. Non-White infants experienced a first-year death rate decline of 0.43 per 1,000 births. Premature infants saw even larger mortality reductions of 1.6 deaths per 1,000 births.
Analysis by cause of death finds that mortality declined most for conditions originating in the perinatal period, such as complications from prematurity and low birth weight. They also find significant declines in mortality due to external and sleep-related causes.
Hospital discharge data from nine states show that, while hospitalization rates did not change significantly, average charges for nondelivery infant hospitalizations fell by $676 per birth—a 19 percent reduction from the sample mean of $3,492. The largest reductions occurred for hospitalizations involving digestive conditions, immune-related illnesses, and conditions originating in the perinatal period.
The researchers provide evidence of several channels through which the hospital support policies may have improved infant health. They find that breastfeeding initiation rose by 4.1 percentage points following policy implementation, a 5 percent increase relative to the pretreatment mean. The share of infants still breastfed at three months increased by 5.7 percentage points (9 percent). These effects were largest for non-White infants, whose breastfeeding initiation increased by 4.3 percentage points (5 percent) and three-month breastfeeding rates rose by 7.7 percentage points (13 percent).
They also show evidence of improvements in infant sleep practices following policy adoption. The researchers argue that this finding, combined with broader changes in household behaviors, such as maternal time spent on childcare, may also play an important role in the observed improvements in infant health.
- Leonardo Vasquez


