Medicare Eligibility Reduces Cancer Mortality for Women
Cancer is the second-leading cause of death in the United States and, because roughly half of newly-diagnosed cancer patients are over the age of 65, Medicare plays a key role in its treatment. In Does Medicare Coverage Improve Cancer Detection and Mortality Outcomes? (NBER Working Paper 26292), researchers Rebecca Mary Myerson, Reginald Tucker-Seeley, Dana Goldman and Darius N. Lakdawalla assess the impact of Medicare eligibility at age 65 on cancer detection and outcomes.
The researchers calculate that the Medicare eligibility age of 65, compared to a hypothetical eligibility age of 66, avoided about 1,800 deaths from cancer at age 65 during their 15-year sample period.
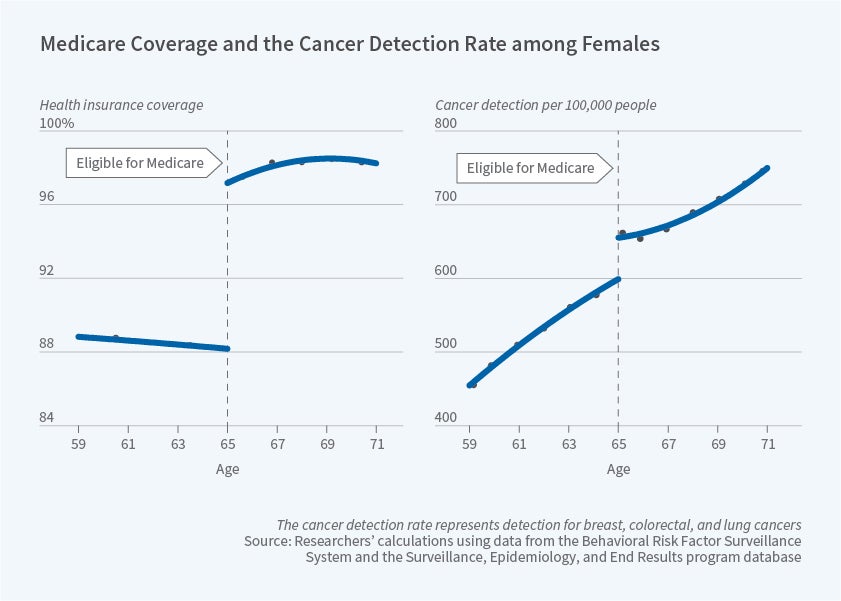
The first panel of the figure shows — for women — the discrete change in insurance coverage that occurs at age 65. The researchers ask whether this change generates a similarly discrete change in cancer outcomes. They assume that, in the absence of the change in Medicare eligibility, rates of cancer detection and cancer mortality would increase smoothly at age 65. As a result, the researchers focus on tumor sites for which screening recommendations are consistent below and above the age of 65: these include breast, colorectal, and lung cancers.
Using data from the Surveillance, Epidemiology and End Results (SEER) program from 2001 to 2015, the researchers show that cancer detection increases discontinuously by 50 per 100,000 people at age 65, a 10% increase compared to average annual cancer detection rates below age 65. Rates of detection rise substantially more for women than for men. Specifically, cancer detection increases by 72 per 100,000 in the female population — as seen in the second panel of the figure — and 33 per 100,000 in the male population.
The researchers turn to Vital Statistics data from the same time period to determine whether the increased insurance coverage at age 65 translates into health improvements. They find evidence of decreased cancer mortality. Consistent with the gender difference in cancer detection results, the cancer mortality improvements are concentrated among women. Specifically, annual cancer mortality decreases by 9 per 100,000 among women, with no statistically meaningful change for men. The improvement in cancer mortality among women is chiefly driven by decreases in mortality related to lung cancer.
The researchers observe racial disparities in cancer stage at diagnosis and in cancer mortality below age 65. They show that access to Medicare coverage at age 65 reduces these disparities among women. The researchers explain that "the disproportionate effect of Medicare on cancer detection and mortality among Black women may reflect the higher proportion of cancers detected at a late stage among Black women prior to age 65 and the larger impact of Medicare on health care utilization and access among racial minorities."
The discontinuous change in health insurance coverage could translate into changes in cancer outcomes for at least two reasons. First, Medicare coverage could affect access to treatment, resulting in treatment changes even for those who were diagnosed with cancer before the age of 65. Second, the earlier detection resulting from the Medicare-coverage-induced rise in screening could lead to more favorable outcomes as a result of earlier treatment.
To confirm the validity of their analysis, the researchers examine the same age patterns in Canada, where health insurance does not change discontinuously at age 65, and find no change in cancer detection or cancer mortality.
The researchers conclude by considering the implications for cancer mortality of potential adjustments to the age of Medicare eligibility. They calculate that the Medicare eligibility age of 65, compared to a hypothetical eligibility age of 66, avoided about 1,800 deaths from cancer at age 65 during their 15-year sample period.
The researchers acknowledge funding from the National Institute on Aging under award 2P30AG043073 and from the Leonard D. Schaeffer Center for Health Policy and Economics. Tucker-Seeley acknowledges funding from a National Cancer Institute K01 Career Development Grant (K01 CA169041).