Prescription Access and Public Health Outcomes
The hepatitis C virus (HCV) is a major public health concern due to its high infection and mortality rates. Recent pharmaceutical innovations known as direct-acting antivirals (DAAs) have the potential to cure HCV and can also generate positive health externalities through reduced transmission. However, the high cost of these drugs—with a sticker price of approximately $84,000 for the course of treatment when initially introduced in 2013—creates substantial obstacles to their use under traditional reimbursement schemes and in cash-strapped Medicaid programs.
In Subscriptions to Prescriptions: Lessons from Louisiana’s Effort to Eliminate Hepatitis C (NBER Working Paper 33617), James M. Flynn, Bethany I. Lemont, and Barton Willage evaluate the effects of the Louisiana Hepatitis C Elimination Plan (LAHCEP). This plan, adopted in 2019, involved an exclusive contract between the state and a pharmaceutical provider of a generic DAA treatment. In return for a fixed annual fee, the firm would provide DAA drugs at no marginal cost to individuals who were covered by the state’s Medicaid program or who were incarcerated. The state’s incentive in maximizing the value received for its payment was to increase the number of hepatitis C patients receiving DAAs. The stated objective was to diagnose 90 percent and treat 80 percent of the state’s residents with HCV.
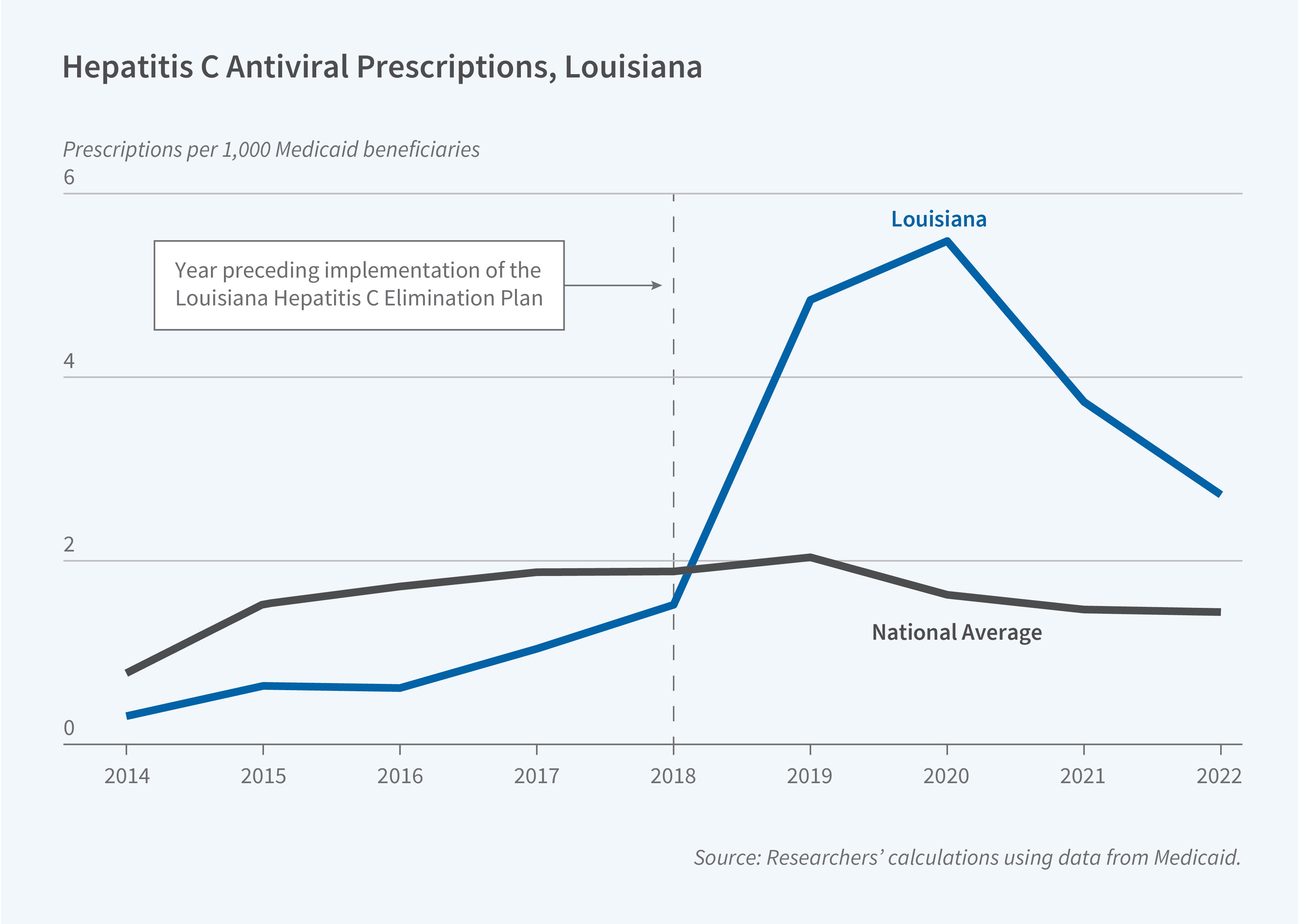
Using data from the Centers for Disease Control and Prevention, the researchers find that implementation of the LAHCEP in 2020 increased HCV diagnoses from 8 cases in 2019 to 281 in 2020, 308 in 2021, and 165 in 2022. Using the Centers for Medicare and Medicaid Services State Drug Utilization Data, they estimate that the plan raised the number of DAA prescriptions per 1,000 Medicaid beneficiaries, which was 1.52 in 2018, by 211 percent in 2019, 270 percent in 2020, 165 percent in 2021, and 96 percent in 2022. By the end of the fourth year of the five-year program, Louisiana had treated over 30,000 patients—67 percent of the state’s estimated HCV-positive population.
The researchers also examine patient-level data from the Scientific Registry of Transplant Recipients. They estimate that the LAHCEP reduced the number of liver transplants in Louisiana by 27 percent and improved the average liver function of wait-listed candidates by 6.5 percent. Data from the National Vital Statistics System show that HCV-related mortality declined by more than 11 percent in the first four years of this program, amounting to more than 300 fewer deaths. This implies that one HCV-related death was avoided for roughly every 85 DAA prescriptions filled between 2019 and 2022. Because of the slow progression of HCV infection, these estimates likely understate the full extent of reduced mortality.
The researchers conduct a back-of-the-envelope calculation to estimate the marginal value of public funds (MVPF) from this program. This is difficult to do without precise data on the cost of surveillance, but they demonstrate that under very conservative assumptions about these costs, the program would pay for itself if each prescription prevented $4,150 in lifetime medical expenses. Meanwhile, previous research has shown that each untreated HCV case leads to approximately $16,000 in medical expenditures each year on average, which suggests the MVPF of this program is large.
— Lauri Scherer


