Racial Concordance and the Take-Up of Preventive Care
Providing preventive care for chronic health conditions has the potential to deliver a rare “win-win” situation in which total costs fall and health care outcomes improve. One of the barriers to such care is mistrust between provider and patient. Such mistrust is one of the factors that can limit the effectiveness of care delivered to Black patients by White doctors rather than their Black counterparts.
In Racial Concordance and the Quality of Medical Care: Evidence from the Military (NBER Working Paper 30767), Michael D. Frakes and Jonathan Gruber assess how racial concordance between patients and medical providers affects the use of preventive care as well as patient outcomes.
Doctor-patient race match is associated with better maintenance of preventive care and better health outcomes.
They analyze a large, geographically dispersed sample of individuals in the military. Three features of the Military Health System (MHS) make it an excellent setting for studying the effects of concordance. First, moves are frequent in the military and they are unlikely to be driven by factors such as health, economic conditions, or race. Second, the MHS provides complete claims data for all care used by MHS enrollees, allowing assessment of concordance impact on both preventive care and follow-up outcomes, including mortality, that may result from differential use of preventive care. Third, because most of the doctors treating patients in the armed forces are also patients themselves, it is possible to use demographic attributes in the MHS database to identify their race.
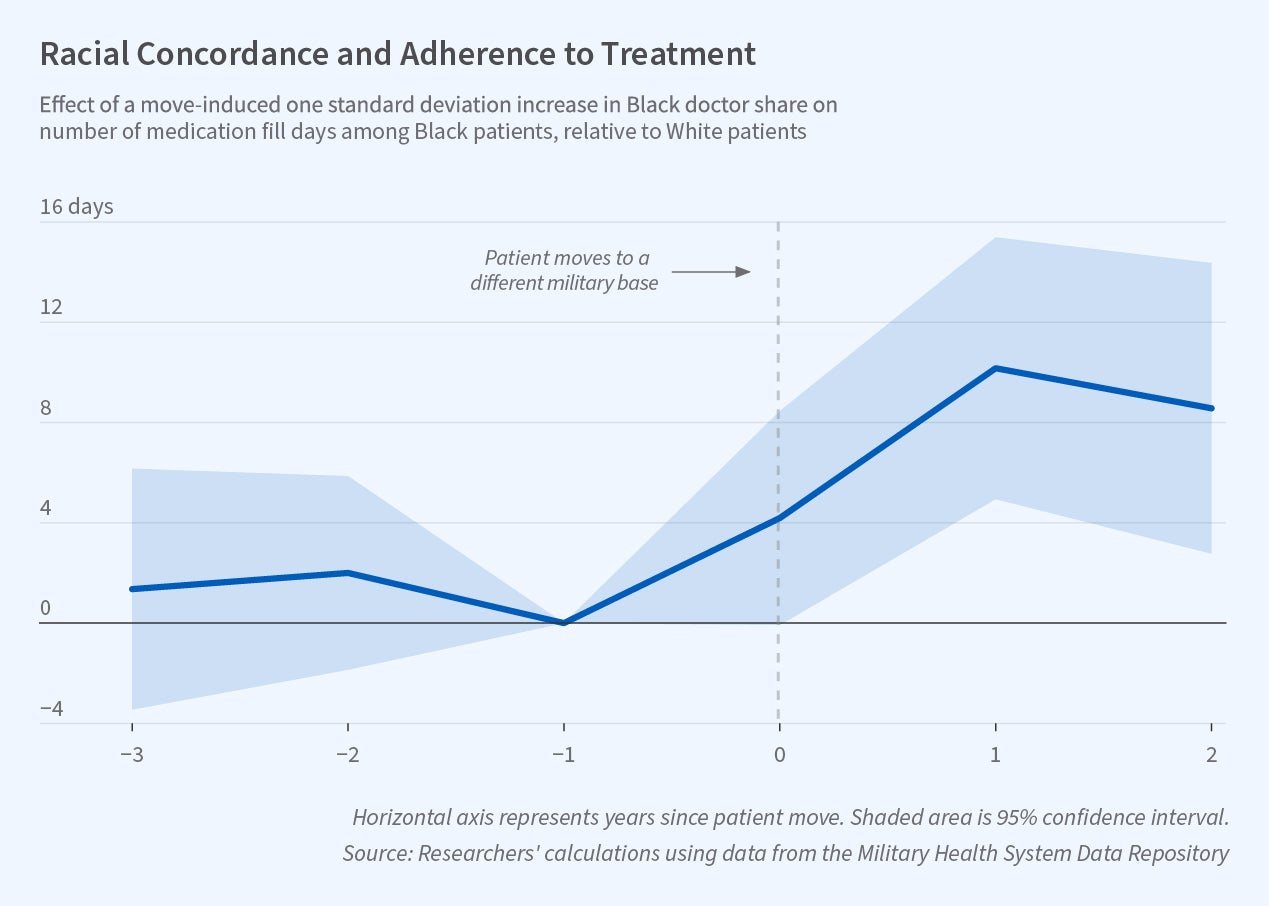
The researchers consider patients with four chronic illnesses: diabetes, high blood pressure, high cholesterol, and clinical atherosclerotic cardiovascular disease (clogged arteries). Though life-threatening, these conditions can be managed with relatively inexpensive medications, diagnostic monitoring, and a range of lifestyle measures. For all four conditions, concordance has a sizable positive effect on preventive care utilization and on health outcomes. Pooling data on all four diseases, the researchers estimate that a 7 percentage point increase in the share of providers who are Black—representing a roughly one standard deviation increase in the share of Black providers across bases—leads to a 15 percent decline in the gap between the Black and White mortality rates for those with these manageable illnesses. More than half of this decrease arises through improved medication use and adherence; other aspects of the provider-patient relationship account for the rest.
The study concludes that provider trust is essential to ensuring adherence with low-cost but life-saving medical treatments, and that efforts to diversify the physician workforce could meaningfully impact the large racial mortality disparity in the United States.
The researchers acknowledge support from the National Institute on Aging under grant R01AG049898.
—Lauri Scherer


