Do Specialists Improve Outcomes for Hospitalized Patients?
Health care provided by specialists is associated with greater treatment intensity than health care by general practitioners, raising questions about the costs and benefits of the additional care. Researcher Joseph J. Doyle, Jr., in Physician Characteristics and Patient Survival: Evidence from Physician Availability (NBER Working Paper 27458), presents evidence that substantiates the higher costs of care by specialists, and shows that this care by specialists benefits patients through reduced mortality.
Doyle’s research focuses on Medicare beneficiaries who were admitted to the hospital through the emergency department with heart failure — the most common reason for this type of hospital admission. The analysis brings together data on the patients’ health care from Medicare claims, mortality from Vital Statistics, and physician characteristics from the American Medical Association’s Masterfile.
Hospitalized heart failure patients are typically treated by general practitioners rather than by specialists. Only 17 percent are assigned a cardiologist as their attending physician and 25 percent are directly treated by a cardiologist. Patients who are treated by a cardiologist tend to be healthier than those treated by general practitioners. They are, on average, one year younger and have 11 percent lower Medicare spending over the year preceding hospitalization. They are also much more likely to be men, with 55 percent of cardiologists' patients being male compared to 44 percent among non-cardiologists. As a result of these baseline differences, a simple comparison of outcomes for patients treated by different types of physicians would be misleading.
Doyle circumvents this concern by focusing on variation in cardiologist treatment that arises solely from day-to-day differences in the staffing mix within a hospital. On average, there are two cardiologists available on the date of admission for patients as observed in the sample, but the exact number varies considerably within hospitals. Thirty-four percent of the patients are admitted on a day when no cardiologists are available at their hospital, while nearly 20 percent are admitted on a day when four or more are available.
The analysis compares patients admitted on different dates, but to the same hospital during the same calendar quarter and on the same day of the week. The key assumption is that any variation in staffing across those dates is not related to patient characteristics. Indeed the data support that premise, with nearly identical observable patient characteristics across different levels of cardiologist availability, including patient age, sex, and prior-year healthcare spending.
As the number of available cardiologists increases from zero to two or more, the likelihood that a patient is assigned a cardiologist as an attending physician increases by 22 percentage points. The likelihood of undergoing a major cardiovascular operation increases by 1.9 percentage points and rates of cardiac catheterization increase by 1.2 percentage points (i.e., 15 percent higher compared to the mean catheterization rate). Medicare spending also appears to be higher, although these estimates are less precise.
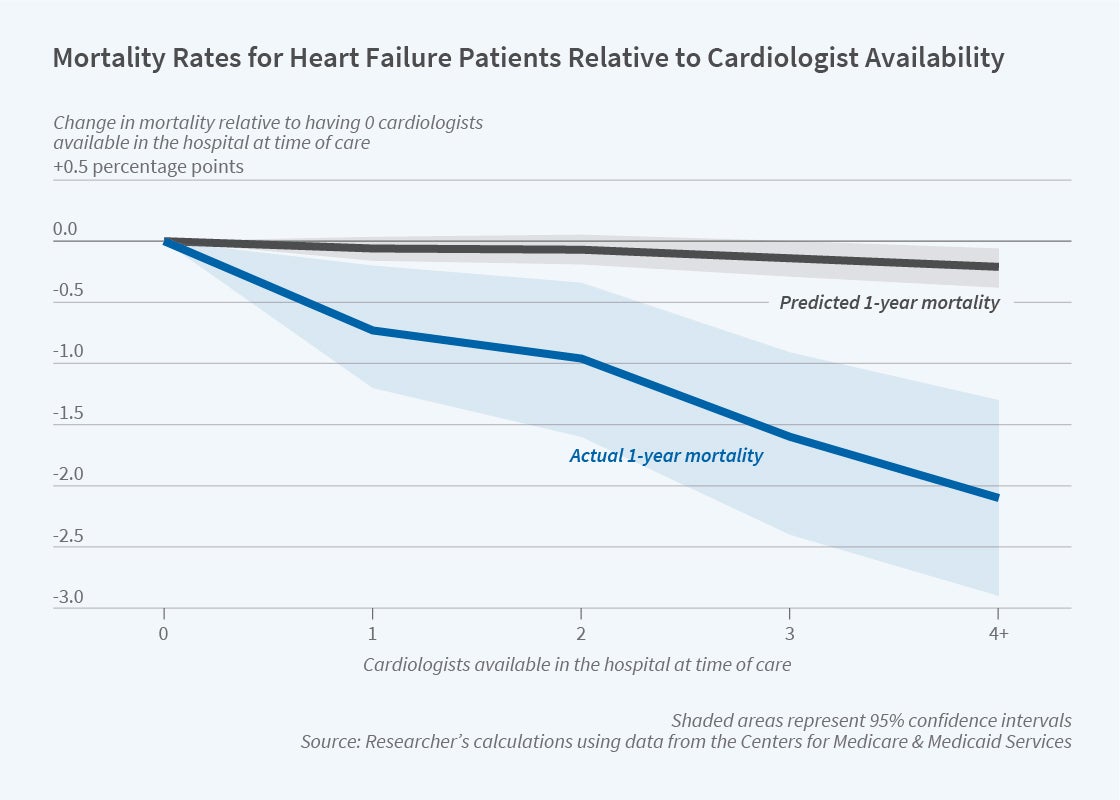
Heart failure patients in the sample face a 36 percent one-year mortality risk, but cardiologist availability lowers this risk. As the figure shows, one-year mortality declines substantially with cardiologist availability. In comparison, predicted one-year mortality — which is based solely on patient characteristics — is largely unrelated to cardiologist availability. Combined with the increase in the use of specialists, these results suggest that treatment by a cardiologist may lower mortality by approximately 7 percentage points or nearly 20 percent compared to the average mortality risk for this group of patients.
The statistical analysis indicates that increasing the number of available cardiologists from zero to two or more results in a 1.2 percentage point reduction in mortality. Doyle infers that specialty care is cost-effective for these patients, with an estimated cost of saving at least one year of life — calculated under strong assumptions — of approximately $50,000.
Doyle extends the analysis of heart failure patients to six other common causes of emergency admissions for Medicare patients, such as strokes and hip fractures. Greater availability of the specialists who are most relevant to these diagnoses is associated with reduced one-year mortality for five out of the six diagnoses. That is, the results for heart failure patients appear to be more broadly applicable. Doyle concludes that Medicare beneficiaries “admitted with common emergency conditions appear to benefit from the availability of specialists.”
The researcher acknowledges support from the National Institutes of Health (Grant R01 AG41794).