Digital Health Technology and Patient Outcomes
Digital health technologies, such as remote monitoring devices and telemedicine services, have attracted considerable interest due to their potential to reduce healthcare costs and improve patient outcomes. These innovations could, however, exacerbate health disparities if adoption rates are lower among underserved communities.
In Equity and Efficiency in Technology Adoption: Evidence from Digital Health (NBER Working Paper 32992), researchers Itzik Fadlon, Parag Agnihotri, Christopher Longhurst, and Ming Tai-Seale analyze a remote patient monitoring program for cardiovascular risk management at UC San Diego Health (UCSDH). The study included 2,512 patients with poorly managed hypertension, referred to the program by their primary care physicians (PCPs) between October 2020 and July 2022. Participants received free Bluetooth-enabled blood pressure devices that transmitted data to UCSDH for daily monitoring by clinical staff.
After one year, average systolic blood pressure had fallen by 9.8 mmHg (from a pre-intervention baseline of 134 mmHg) for patients who were referred to the program. Since only 53 percent of the patients who were referred to the program actively participated in it, the implied impact on systolic blood pressure for participants is a reduction of 18.5 mmHg.
Within one year, patients who were referred to the program were 15 percentage points more likely to reach healthy blood pressure levels (below 120 mmHg). The program also reduced the share of referred patients at high risk for severe cardiovascular events by 4.4 percentage points, a 12.4 percent decrease from the baseline. By three quarters after referral, the intervention reduced quarterly healthcare costs by $385 per referred patient, a 40 percent decline from a predicted level of $1,004.
The researchers hypothesize that these outcomes were driven by better-tailored medication regimens and patient behavioral changes. Participants experienced a temporary increase in unique prescription orders, particularly in the first quarter, suggesting experimentation to find more effective medication. Additionally, in a subsample of 204 referred patients for whom information on smoking behavior was available, the intervention was associated with a persistent reduction in smoking, consistent with improvement in healthy behaviors.
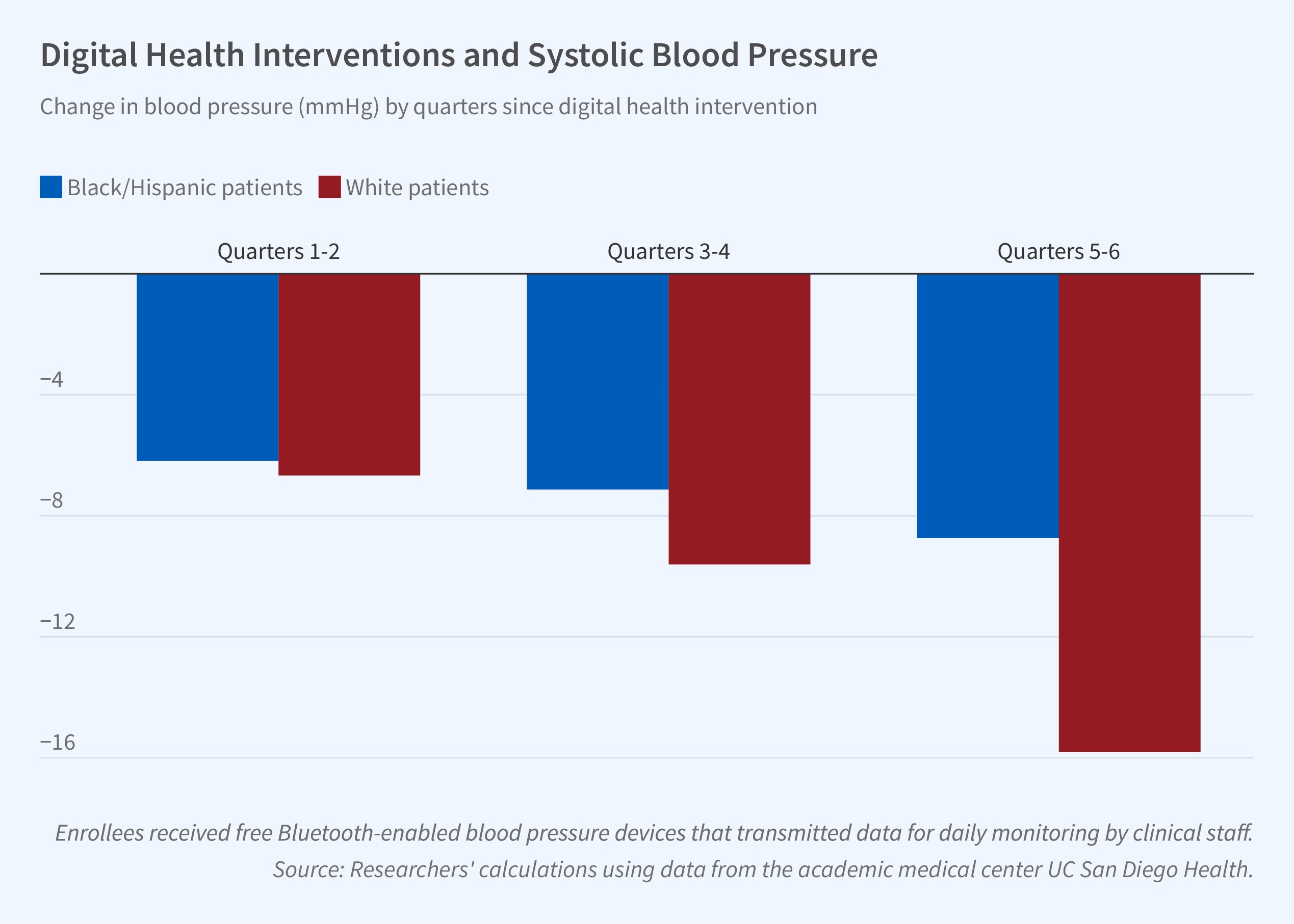
The intervention generated unequal gains in health outcomes. By the end of the study period, White patients experienced nearly double the blood pressure reduction (15.81 mmHg) of Black and Hispanic patients (8.74 mmHg). Similarly, patients from more advantaged communities saw greater reductions (14.85 mmHg) than those from less advantaged areas (8.62 mmHg).
One explanation for the disparities is the difference in continued participation over the 18-month sample period. By the end of the study period, the participation rate among Black and Hispanic patients who were referred to the program was 4 percentage points lower than that for Whites, suggesting that the former groups may face greater barriers to continuous engagement with the program.
The study finds that PCPs can be influential in patient participation and continuation. Patients of high-performing PCPs, as measured by their tier in a pay-for-performance system, had a 10.5 percentage point higher average participation rate over the study period than patients of the lowest-performing PCPs. Additionally, longer physician-patient relationships were associated with an increase in program participation. Strengthening physician-patient relationships could therefore be a pathway to promoting greater and more equal engagement with digital health technologies.
— Leonardo Vasquez


