The Effect of Wait Time Targets in Emergency Departments
Emergency departments (EDs) face the complex challenge of serving patients who arrive with a wide array of problems, some life-threatening. ED nurses and physicians must quickly decide which patients must be seen immediately and which can wait. They must also decide which diagnostic tests and procedures to perform in the ED, as well as when to admit a patient to the hospital and when to send them back home.
Long ED wait times are an increasing focus of public attention. In some U.S. cities, there are digital billboards advertising current wait times at local EDs. Several nations have introduced financial rewards or penalties for providers based on ED wait times.
The effects of policies that encourage shorter ED wait times are not well understood. One concern is that such policies could lead providers to make decisions that compromise the quality of patient care. On the other hand, it is not clear whether providers fully take into account the effect of wait times on patient outcomes in the absence of these policies.
In Saving Lives by Tying Hands: The Unexpected Effects of Constraining Health Care Providers (NBER Working Paper No. 24445), researchers Jonathan Gruber, Thomas Hoe, and George Stoye explore the effect of the imposition of a "four-hour wait" policy in England.
Implemented in 2004, the policy required 98 percent (later 95 percent) of patients to be discharged, admitted as an inpatient, or transferred to another hospital within four hours of arrival. Meeting the target is a key factor in the evaluation of overall hospital performance, with managers at risk of being fired for poor compliance. Further, the financial penalty for missing the target is more than twice the average revenue of an ED patient, with total fines equaling one-third of hospital deficits. To help them meet the target, EDs have adopted IT systems that track patient wait times and hired staff to monitor wait times and alert physicians when the four-hour threshold is approaching.
The analysis uses administrative records of 15 million visits to EDs at public hospitals from 2011 to 2013. These data include detailed information about ED visits and any subsequent care received during an inpatient stay, and are also linked to national mortality records.
There is a large spike in wait times at the four-hour mark, with a patient's visit to the ED 2.5 times more likely to be completed in the 10 minutes before the cutoff than in any other 10-minute window. The researchers use a "bunching estimator," first developed to study the effect of tax rate thresholds, to estimate the counterfactual distribution of wait times that would exist in the absence of the four-hour policy. They find that the policy reduced wait times for impacted patients by nearly 20 minutes, or 8 percent.
Turning to how the policy affects treatment decision and outcomes, the researchers develop a method that allows them to distinguish the portion of the spike at the four-hour mark which results from providers treating sicker patients more quickly (the "composition" effect) from that which results from changes in provider behavior (the "distortion" effect). The latter is the finding of interest.
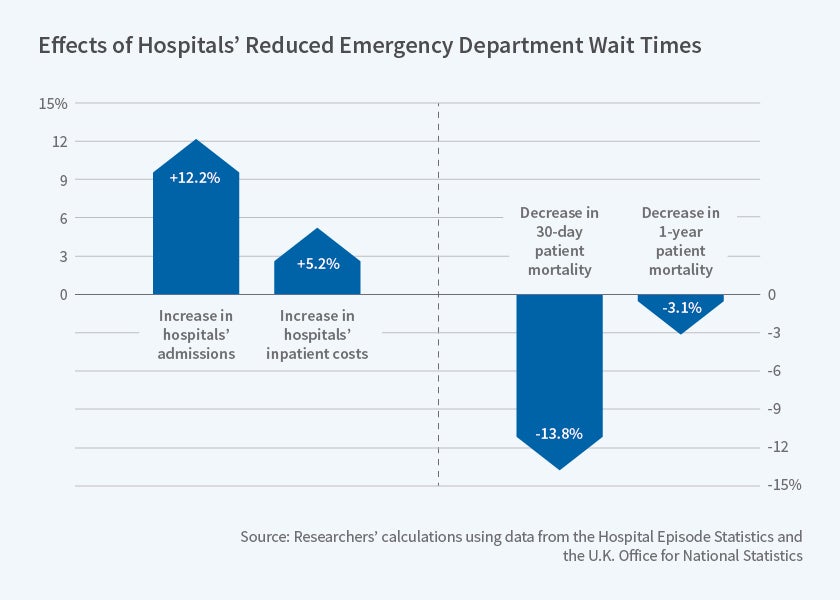
The researchers find that the policy leads to more intensive testing of patients in the ED and a modest increase in ED costs. The policy also leads to a 12 percent increase in the probability of inpatient admission and a corresponding decrease in discharges to home. While these marginal inpatients use relatively few resources during their stays, the extra visits are nonetheless associated with a 5 percent increase in payments from the government for inpatient services.
Interestingly, there are significant gains in patient outcomes from the policy — the 30-day mortality rate is estimated to fall by about 14 percent for patients affected by the policy, while the one-year morality rate falls by about 3 percent. The researchers note that these effects are large relative to the effect on spending, suggesting a cost of extending life by one year of $43,000.
Overall, the findings indicate that the policy induced EDs in England to reduce wait times and increase inpatient admissions, resulting in cost-effective mortality improvements. This suggests that provider decisions in the absence of the four-hour policy would not be optimal. Cautioning that their results might not apply in other contexts with different wait time limits or incentives for compliance, they conclude "more work is clearly needed to understand the proper set of rules and incentives for delivering cost-effective ED care."
Hoe and Stoye acknowledge financial support from the UK Economic and Social Research Council through the Centre for the Microeconomic Analysis of Public Policy (CPP) at IFS.